
How to build a successful diagnostic device
September 2021
By Craig Townsend – Director of Healthcare at 42 Technology

Recent reports, including The Future of Diagnostics Delivery Report backed by the Institute of Biomedical Science (IBMS) and the Association of British HealthTech Industries (ABHI), call for significant funding in diagnostic innovations.
This is largely due to the current disparity between the value diagnostics deliver to the health system and the investment they receive. Numerous human factors are also increasing the demand for Point of Care testing including the increase in infectious diseases in developing countries, the rapid rise in lifestyle diseases such as cardiac diseases and diabetes and technological advances in molecular testing.
The evidence is clear, the world needs better quality and more readily available diagnostics, especially those that can be used in a home environment. This is the current commercial and altruistic opportunity facing many start-ups and established companies. So what is the process behind diagnostic development? And how can you build something commercially successful?
What is a diagnostic device?
Not everyone is familiar with the diagnostics market. What is meant by the term 'diagnostic device'? Diagnostic devices, also known as in vitro diagnostics (IVD) products are instruments, reagents and systems used to test whether a person has a disease or other condition. Such products are intended for use in the collection, preparation and examination of specimens taken from the human body. The most well-known diagnostic is probably the home pregnancy test, but tests exist for HIV, hepatitis, diabetes monitoring, tuberculosis - pretty much all known disease types - which helps highlight the importance of diagnostics.
There is one more subclassification for diagnostic devices known as Point of Care (POC). Diagnostics are often conducted in laboratories, equipped with specialised tools and trained personnel. You, the end user, supplies a sample to be tested. This sample is stabilised, managed and taken to a lab to be processed. You then get results of your diagnostic test after a few days (depending on logistics).
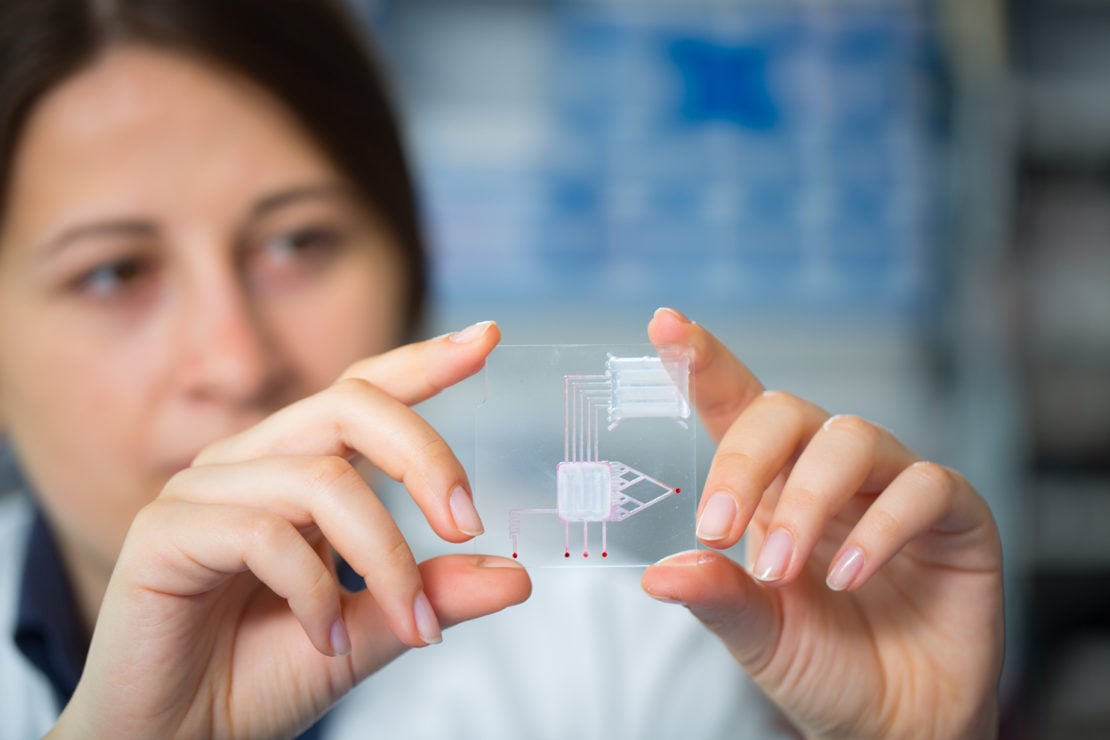
Think of a routine blood test, where you visit a location. Someone takes a sample and sends it away. You then receive results within a few days. POC significantly reduces the amount of time needed to get a result. It provides a result at the ‘Point of Care’. The chemistry is handled on the device itself, without the need of specialist equipment or personnel and presents a result direct to the end user within minutes. The home pregnancy test is an example of a diagnostic device, but more specifically it’s an example of a POC diagnostic. You provide your sample and get a result in minutes without ever having to leave the house.
Key stages of diagnostic development
Now that we have seen the market demand for better diagnostic devices and better classified what we mean by diagnostic devices, how do you go about starting development? I have broken things down into four simple steps:
Step 1: Planning and Strategy
I have seen some ground-breaking technology fail because it lacked a quality commercial strategy. Keep asking yourself these three questions: What? Why? Who?
- What is the intended use of this product?
- Who is this product for?
- Why would someone use this product instead of a competitor product?
- Who else has a similar product?
- What is our differentiator?
Without a strong commercial strategy, you could spend a lot of time and money developing something that already exists or that nobody wants. It sounds simple, but my time spent in Venture Capital taught me that strategy is often second place to ‘cool idea’.
If you would like support with your commercial planning, or you just want a sounding board to bounce ideas off, you can always reach out to 42 Technology to start the conversation.
Your commercial strategy will also lay strong foundations for your regulatory strategy, which you should also establish at the start of your project. Much like medical devices, diagnostic devices are also regulated by the Food and Drug Administration (FDA) in the USA, Medicines and Healthcare products Regulatory Agency (MHRA) in the UK and varying European Medicines Agency (EMA) member states in Europe, although criteria differs.
It’s important to understand the specifics associated with your diagnostic device. So look at product literature from your competitors or similar devices to determine the types of testing you will be required to pass and the volume of data these bodies expect you to submit.
Your chosen regulatory strategy can have a big impact on the best approach for technology development, and vice versa. Partner early with a specialist consultancy to help plan your programme to gather the right evidence at the right time.
Step 2: Assay Development

You have developed a laboratory assay with the required sensitivity and specificity. Everything works in the lab, and you are confident that your test works. You’re halfway there! Or so it seems… but this is a long way from a commercially viable product. Packaging the assay, taking it from a multistep process carried out by an expert, to something semi or fully automated is not an easy task, mainly due to real world factors reducing the sensitivity and specificity values provided by the development scientists. There will be a point during development where you hit a point of compromise.
Start by deconstructing the assay workflow. Identify steps and boundaries to identify critical steps versus those idiosyncrasies of the lead scientist. When reviewing protocol and conducting our own testing, we often find that critical steps are also missing, or seen as redundant, such as shaking the sample. Previously, we have had our engineering team observe assay scientists to extract vital insights and build a development brief that includes:
- What is the most appropriate detection modality?
- What are the reagent requirements and how will they be stored?
- What impact will usage scenarios have and what will this mean for liquid handling requirements?
Understanding the conditions and workflows required for acceptable assay performance is key when trying to contain it within a diagnostic device which leads to step three, the device itself.
Step 3: Device Development
Your assay needs to be contained and defining system architecture is a crucial task. Consider the following:
- Who is the end user?
- How will they interact with your device?
- What are the usage scenarios?
- Will the device test a single sample, or will there be batch testing?
Depending on your answer to these questions, your commercial, technology and device strategy may have to differ. For example, you could have a simple instrument that requires the end user to complete a number of complex tasks in order to achieve the desired outcome. This could result in a relatively simple to manufacture device, with a huge margin of user error affecting performance.
Alternatively, you could produce a more automated device that reduces user error. But this could increase the cost of development, slow down go to market and incur lengthy approval times from regulators. The utopia is of course something simple to use, cheap to manufacture and with a high level of accuracy, but compromise often has to take place.
Not all diagnostic devices have to be simple to use and fit in the palm of your hand. But speaking with a specialist about optimising your approach is a good first step in reaching your utopia.
Step 4: Usability and Testing
Usability should be considered at every point of your design process, but I feel it warrants its own step, given the importance of the IEC 62366 standard. It’s incredibly important to achieve an enhanced user experience whilst minimising the risk prevalent with all medical devices. As I mentioned previously during Step one, a technically outstanding product with a poor commercial strategy is likely to fail. Exactly the same can be applied to an outstanding product with poor usability.
The best way to ensure good usability, is to create a detailed task analysis, once the system architecture has been defined. This starts with the analysis of the assay steps performed at the outset of the development program and understanding the impact of the usage scenario on how the user will perform various steps and interact with the device. This process ensures continual iteration and optimisation throughout development.
The 'next big thing'
Whether you are attempting to prevent and control the spread of infectious disease, or helping people make informed lifestyle choices, diagnostics are a vital part of everyday life. Prevention is not only more cost effective than cure, it also enables better planning and treatment management and therefore the ‘next big thing’ is in the field of diagnostics.
When planning your new diagnostic venture, consider the following:
- Build a strong strategic plan, addressing market need, idea validation and competitive landscape
- Plan for regulatory approvals early on, research competitor approvals and assess how much evidence will be required to gain approval
- Construct a development brief for your assay, ensuring that all processes are captured - no matter how insignificant!
- Define your system architecture and map out your customer profile. How will they interact with the device?
- Perhaps most importantly when starting a new venture, bring on the right expertise as and when required
42 Technology is a specialist in the field of diagnostic development and has been working with global diagnostics specialists and non-profit organisations for the past 12 years, to bring a wave of diagnostic innovation to market.
You can also read more about our work here: What we do

If you would like to find out more please contact Craig:
craig.townsend@42T.com | +44 (0)1480 309461 | www.linkedin.com/in/craig-c-townsend
Craig is a management and product consultant, specialising in Healthcare and Life Science. For the past 13 years, Craig has been working with some of the world’s leading brands and most exciting start-ups to bring a new wave of technology innovation to market, solving complex problems primarily in medical devices and wearables.
Craig has an MBA from the CASS Business School at City, University of London and is an active angel investor across a number of digital therapeutic start-ups, after exiting his own start-up in 2018.
Share this article:
Related Articles

Healthcare & Life Sciences
The future of home healthcare: trends and innovation

Healthcare & Life Sciences
Right to repair: reshaping the medical equipment industry

Healthcare & Life Sciences
The hidden risks with smart injectors - is high-tech sacrificing usability?

What will you ask us today?
We believe in asking the right questions to drive innovation; when we know the right questions, we generate the ideas to answer them.

