
Osteoporosis – a silent burden
November 2022
By Marta Uncio Ribera, Biomedical Engineer at 42T
As I highlighted in my previous article 'Women's health: data bias in healthcare', there are numerous conditions that affect men and women differently or disproportionately. Osteoporosis is one of them.
Osteoporosis is a bone condition that is caused by increased levels of bone loss which reduces bone density, weakens bones, and can lead to fractures. It is estimated that it affects 200 million people worldwide. Age and being female are two of the main risk factors – 80% of Americans with osteoporosis are women and it affects 1 in 4 women over 65.

It is often referred to as a silent disease as it develops gradually over time and is often symptomless until a fracture occurs. Every year in the UK alone, it causes half a million fractures and costs the NHS £4.6bn. And with an aging population, this will only get worse.
What causes osteoporosis?
Throughout our lifetime, our bones are continuously being renewed through a process called remodelling. This process is driven by the activity of two types of cells in our bones – osteoclasts and osteoblasts – which are responsible for bone resorption and deposition respectively.
Osteoporosis occurs when there is an imbalance between these two activities and the rate of bone formation does not match the resorption rate. This imbalance reduces bone mineral density and therefore makes bones more brittle and prone to fracture.
How the bone remodelling process is regulated is highly complex, but hormones like oestrogen, parathyroid hormone, and testosterone play an important role in maintaining bone mass. Peak bone mass is achieved by the mid-twenties, but it then gradually declines with age.
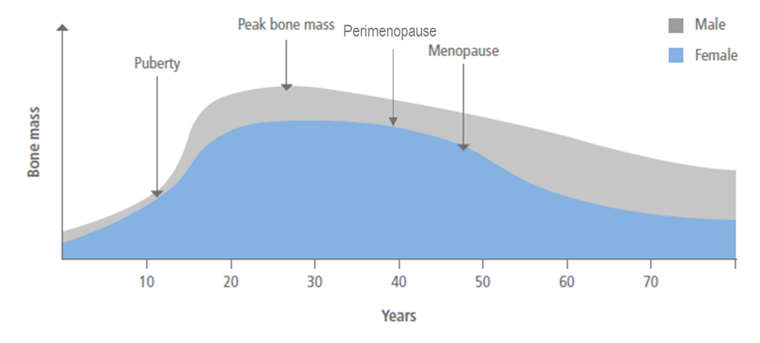
Figure 1 – Bone mass throughout the life cycle
Osteoporosis is a disease that affects both men and women, but the latter are affected disproportionately. Whilst in men, bone mass slowly decreases with age, in women, the drop in oestrogen levels after menopause can lead to a quick and significant decrease in bone mass (see Figure 1).
Current diagnosis options
The most common method to diagnose osteoporosis is dual-energy x-ray absorptiometry (DXA). This technology measures the attenuation of low radiation X-ray beams of two different photon energies to calculate bone mineral density (BMD). There are a few other imaging methods available to measure BMD, such as quantitative computer tomography (QCT) or quantitative ultrasound (QUS), but their clinical uses are more restricted.

BMD is used to assess the risk of fracture but as the symptoms of osteoporosis are not obvious, deciding whether a test is required relies on the evaluation of other risk factors and the person’s medical history.
An easy win in terms of fracture prevention could be achieved by introducing more rigorous testing and screening programs. For example, fracture prediction algorithms such as FRAX® developed by the University of Sheffield, can be used both with and without BMD data to assess the 10-year probability of having a major osteoporotic fracture.
Current treatment for osteoporosis
Once a patient is diagnosed with osteoporosis there are several available pharmacological treatments that can be prescribed to decrease fracture risk. These can generally be divided into two categories, anti-resorptive agents which include oestrogen in hormone replacement therapy, and anabolic agents. But one of the main challenges is assessing treatment efficacy and adherence.

Bone turnover markers (BTMs) which can be measured in the blood or urine can provide a useful insight into these challenges. For example, a significant change can be seen after a few weeks of antiresorptive treatment whilst it can take 1-2 years for a change to be identifiable with DXA.
In addition to the existing medications, patients are advised to make some lifestyle changes, like taking calcium and vitamin D supplements or doing more weight-bearing exercises, which are known to have a positive impact on bone health. The stresses and strains that muscles exert on bones are thought to be a stimulus in the bone remodelling process.

Increased muscle strength and therefore greater forces can stimulate bone formation and therefore help reduce the rate of bone loss. This, together with better coordination and confidence reduces the risk of fracture.
Opportunities for new medical devices
Prevention
Given the lack of symptoms, it is easy for osteoporosis to go unnoticed and cause a fracture. This can significantly affect someone’s mobility and overall health. There is therefore a big opportunity for improvements to be made in the prevention of this silent disease. Medical devices such as Bone Health Technology’s vibration belt could for example help delay the onset of osteoporosis.
This device applies gentle vibrations to the hip and spine. These simulate the mechanical stimuli bone experiences during exercise and can help reduce bone loss.
Diagnosis
Although DXA is the current gold standard for diagnosing osteoporosis it has several shortcomings. For instance, T-scores, which are one of the metrics used to assess fracture risk, are not equally reliable across different populations. DXA also produces a 2D image, so the BMD is calculated based on the area rather than the volume and therefore means that the BMD estimated is affected by bone size.
Alternative imaging methods like QCT can be used to calculate volumetric density but the higher levels of ionizing radiation and the cost currently makes it a less suitable option. In comparison, QUS is safe and much cheaper and might also be able to provide other structural information in addition to bone mass. Several lightweight, handheld ultrasound devices, have been developed in recent years. Although the results are promising, these sorts of devices are yet to be introduced in standard diagnostic pathways. They do not currently provide enough improvement on current methods.
Monitoring
Monitoring BTMs could help ensure patients are treated in a way that is effective for them. But this might have other applications beyond pharmacological treatment monitoring. By tracking someone’s BTMs over time with at-home IVD testing, perhaps the benefits of preventative measures such as load-bearing exercises or vibration devices could be quantified. Developing accessible, point-of-care testing solutions such as quantitative lateral-flow assays could help tackle this global challenge.

Where to from here?
Given the potential economic and health impact osteoporotic fractures could have as the population ages, it is important to work to improve diagnostic and treatment options. The reliability of existing diagnostic methods needs to be improved. For example, by expanding their uses to more skeletal sites or validating them for both men and women across different populations.
There is a huge commercial opportunity for medical device manufacturers, from IVD tests to QUS imaging technologies and preventative wearable devices. Developing these new technologies will help us tackle this silent burden.

If you would like to find out more please contact Marta:
answers@42T.com | +44 (0)1480 302700 | LinkedIn: Marta
Marta is a biomedical engineer with a mechanical background. Along with a wide set of technical skills, she has experience in medical device R&D. Marta graduated with Distinction from the Biomedical Engineering MSc at Imperial College London, specialising in biomechanics. She also holds a mechanical engineering degree from the University of Cambridge.
Share this article:
Related Articles

Healthcare & Life Sciences
The future of home healthcare: trends and innovations

Healthcare & Life Sciences
Right to repair: reshaping the medical equipment industry

Healthcare & Life Sciences
The hidden risks with smart injectors - is high-tech sacrificing usability?

What will you ask us today?
We believe in asking the right questions to drive innovation; when we know the right questions, we generate the ideas to answer them.

