
Why the healthcare industry should focus more on menopause issues
January 2023
by Michaela Hume, Engineer at 42T
Almost a million women have left the workforce due to lack of support during menopause. Suicide rates for women aged 45 - 54 have risen by 36% in twenty years. Misdiagnoses are also common. With stats like these, menopause is clearly affecting a huge proportion of the population. What help is currently available and what more can be done?
What is menopause?
Menopause is reached 12 months after a woman’s last period and is caused by reduced levels of oestrogen production. Perimenopause is the period leading up to this point in time where the hormonal changes are causing symptoms, but menstruation is still occurring, albeit irregularly.
The menopause experience is different for every woman. This includes:
- The age menopause begins, which is usually between 45 and 55 years, but could be earlier or later due to natural causes, uterus/ovary removal or treatments such as chemotherapy.
- The duration of the perimenopause stage, which is often around 7 years but could be up to 14 years.
- And the types, range, and severity of associated symptoms.
Symptoms of menopause can manifest physically and psychologically. Low hormone levels post-menopause also results in increased health risks.
| Physical Symptoms | Mental Health Symptoms | |
| • Hot flushes and night sweats | • Increased anxiety | |
| • Worsened headaches and migraines | • Low mood | |
| • Changed body shape | • Depression | |
| • Dry skin surfaces, dry hair, mouth, and eyes | • Mood swings | |
| • Thinning of hair on the scalp and increase in facial hair | • Problems with memory and concentration (brain fog) | |
| • Heart palpitations | ||
| • Joint stiffness | ||
| • Urinary incontinence | ||
| • Indigestion, nausea, and bowel changes |
| Increased Health Risks |
| • Bone weakening (osteoporosis) - can cause impaired mobility and chronic pain, with hip fractures alone costing ~£2 billion annually. Check out our article. |
| • Cardiovascular disease - 2nd highest cause of death in women; ~16% in 2018 |
| • Poor muscle power and tone - can reduce coordination and further increase fracture risk |
| • Alzheimer's disease - the leading cause of death in women; ~35% of deaths in 2018 |
Why is menopause such a problem?
51% of the population will experience menopause in some form, therefore everyone will either experience it themselves or know someone affected. The prevalence combined with wide range of symptoms, both physical and mental, can affect both personal and professional life, make menopause a difficult period for many women.
| In the Workplace |
| • Poor employer awareness of Health and Safety and Equality Law |
| • The subject is still largely taboo - 47% of women who took a day off due to symptoms withheld the cause of absence |
| • 92% of women reported their symptoms affects their work |
| • Lack of support causes many women to cut back their hours and 900,000 have left work completely |
| • Women of menstrual age and above are the fastest growing group in the workforce - an increase of 30% in 30 years |
| At Home |
| • Suicide rates for women aged 45-54 has risen by 36% in 20 years (2001-2021) |
| • Menopause effects can put a strain on personal relationships |
| • GP help for diagnosis and symptom support is lacking - women who asked for help from perimenopause (39%) and menopause (27%) symptoms, were told by their GP to learn to live with the symptoms. This is corroborated by GPs, 77.5% of whom feel that extra training is required in this area. |
Additionally, the stigma associated with menopausal symptoms, relating to underlying ageist and sexist attitudes, can cause embarrassment. This can further worsen mental health symptoms linked to the decreased hormone levels, worsened sleep due to physical symptoms and body changes.
Diagnosis
The changes in menstrual patterns, along with the displaying of relevant symptoms, at the expected age are thought to be enough to diagnose the beginning of the perimenopausal stage; in the NHS, doctors primarily use a woman’s symptoms, menstruation pattern and medical history to diagnose menopause. It is however difficult to confidently confirm this diagnosis due to complications such as whether a woman takes a contraceptive pill or has undergone a hysterectomy for example. Blood or urine tests can be used to measure follicle-stimulating hormone (FSH) levels as elevated levels can be indicative of menopause.
However, this test is not an approved diagnostic pathway in the UK as the result does not guarantee an accurate diagnosis, particularly if the results are evaluated in isolation; the Royal College of Obstetricians and Gynaecologists (RCOG) advised against the use of FSH over-the-counter urine tests for this reason. The variation in sufferer age, symptoms presented and the added effect of medications such as the Pill can lead to misdiagnosis. Five common misdiagnoses are depression, chronic fatigue syndrome, irritable bowel syndrome, fibromyalgia, and cystitis/thrush.
Symptom Treatment
Pharmaceutical solutions
Hormone replacement therapy (HRT) is the main treatment that can be offered to women suffering from menopause symptoms. As the therapy elevates low oestrogen levels, it can alleviate a large range of the symptoms. It is important to work out the best dosage and delivery method with a doctor to get the most benefit relative to potential side effects. HRT delivery methods include skin patches, gels, implants, or tablets.
Other treatments are available to target specific symptoms. This includes non-hormonal medicines to help with hot flushes and night sweats and drugs or supplements to help with bone-strengthening. Anti-depressants or cognitive behaviour therapy (CBT) may be prescribed to assist with some of the mental health issues.
Alongside these treatments, general lifestyle changes are also recommended. This includes moving to a healthier diet, regular exercise and cutting back on caffeine and alcohol.
Tech solutions
Existing technology focuses on either temperature regulation to target hot flushes or apps such as the ones summarised below.
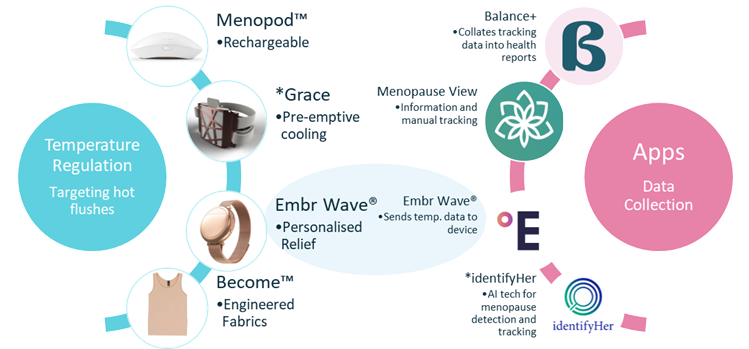
Figure 1: Existing technologies for menopause. *devices/apps still in development or data collection phases. Images: BalancePlus app, Menopod, LadyCare, Grace, Embr wave, Become clothing, Menopause View, identifyHer
The devices are all relatively new – some are yet to launch. Some apps have also been developed for manual symptom tracking and for user control over a temperature regulation device like the Embr Wave®. A promising device, identifyHer, is an app-activated, AI-operated sensor; users wear the sensor for three months, tracking their symptoms, and the sensor collects data which will be provided to their general practitioner. It is intended that the device will allow GPs to make more informed decisions when diagnosing menopause or evaluating current treatment efficacy.
The medical device industry has many opportunities to help improve the current understanding and treatment of menopause…
Evidently, great innovations have been developed in recent years with a general focus on temperature regulation and symptom tracking. There is however significant room for further development.

Potential opportunities for device development can be split into three groups:
- Symptom management
For symptom management, symptoms outside of temperature regulation have been largely neglected.
- Ease of diagnosis
The IdentifyHer device is an example of how our contribution can aid GPs in both their understanding of menopause and their confidence in diagnosis. Another important benefit of monitoring devices is to instil greater confidence in the current available treatments; 80% of menopausal women experience symptoms but the proportion of women on HRT, whilst increasing in recent years, is comparatively minimal – in some UK areas only 10% are on it! It is possible that an improved understanding of HRTs efficacy, particularly on an individual level, could encourage more women to try the treatment with more confidence that its efficacy for them personally can be reliably assessed via continuous monitoring.
- Prevention of related diseases
Diagnostic, screening, monitoring and treatment devices for related diseases is a less ventured space which holds numerous opportunities, particularly at-home devices which can collect data over a longer time and provide context to clinicians.
For example, it known that 50% of future hip fractures will originate from the postmenopausal population who have a prior fracture history, so designing early-intervention devices that can continuously monitor or treat this population to provide preventative care before dangerous fractures occur can only be beneficial on both an individual and societal level.
But the current screening method uses bone mineral measurements to estimate bone strength, which requires technologies dual-energy X-ray absorptiometry (DXA)… validated and accurate but not the most portable.
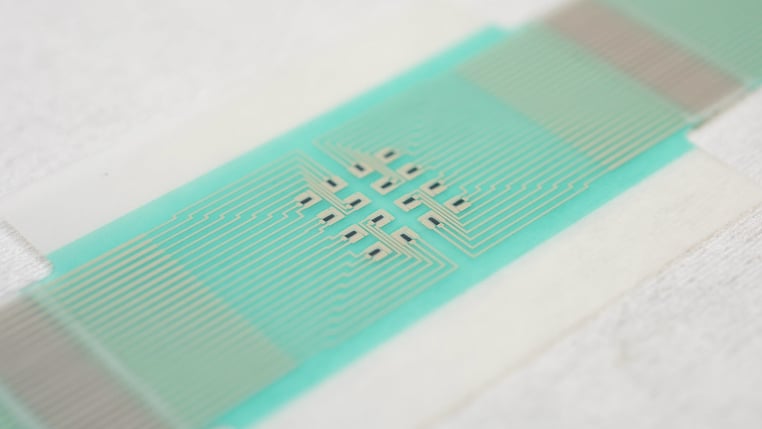
Figure 2: Non-invasive, adhesive patch used to measure glucose levels
Testing for blood-based markers that are indicative of bone turnover can aid diagnosis and monitoring but there are limitations to their use in isolation - they can indicate other conditions. Opportunities could exist to develop sensors inserted under the skin that detect multiple markers, or even non-invasive monitors.
We could take inspiration from innovation within the glucose monitoring sector to meet this challenge, such as advances in microfluidics - adhesive monitoring patches and Lab-on-chip saliva tests are just a couple examples amongst numerous others.
Where can we go from here?
The FemTech industry has come a long way and is fast growing, however most of the industry currently focuses on pregnancy, breastfeeding, and reproductive health; only 6% of FemTech companies focus on menopause issues despite 45% of all women being menopausal and postmenopausal. This shows that vast opportunities still exist for new and established medical device companies to have a real impact in this space.
As a team of engineers and scientists working in healthcare, we love to solve problems which can improve people’s lives and there is a wealth of challenges associated with producing reliable, affordable, at-home monitoring devices that we'd be excited to help you overcome.
We bring deep experience in developing a wide variety of personal care products and medical devices. Examples include diagnostic platforms that utilise microfluidic and other technologies, new sensor technologies, and drug delivery devices.
If you would like to find out more, please contact 42T’s Craig Townsend, Director of Healthcare: craig.townsend@42T.com | +44 (0)1480 302700 | LinkedIn: Craig
About the author:

Michaela holds a first-class Masters degree in mechanical engineering from the University of Bath. She has varied engineering work experience in defence and pharmaceuticals.
Share this article:
Related Articles

Healthcare & Life Sciences
How to rescue medical devices from component problems


Healthcare & Life Sciences
Innovations and future tech spotted at this year's MEDICA event

What will you ask us today?
We believe in asking the right questions to drive innovation; when we know the right questions, we generate the ideas to answer them.


